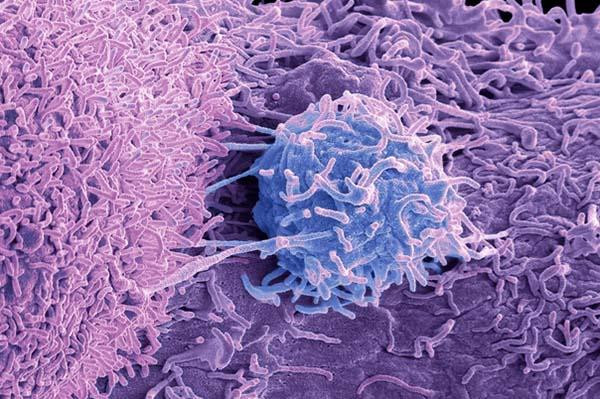
Most men over 50 will develop an enlarged prostate. Also called benign prostatic hyperplasia (BPH), this bothersome condition makes it hard to urinate and can eventually lead to other problems, such as infections, kidney stones, and bladder damage, if left untreated. Many different BPH therapies are available, including medications and various types of surgery.
One of the newer surgical options, called aquablation, trims excess prostate tissues with highly pressurized jets of saline. Doctors perform aquablation in the operating room while looking at the prostate gland on an ultrasound machine. Patients are put under general anesthesia, so they don’t feel any pain during the procedure.
Men typically have to urinate through a catheter for about 24 hours after surgery until swelling of the urethra (the tube through which urine flows out of the bladder) subsides. Aquablation is gaining in popularity — in part because, unlike other more traditional BPH treatments, it can preserve normal ejaculation.
In September, researchers published a study showing that improvements in urinary function from aquablation were still holding up after five years.
Results of data analysis
The study assessed long-term data from two clinical trials. The first, called the WATER trial (for Waterjet Ablation Therapy for Endoscopic Resection of Prostate Tissue) launched in 2015 and enrolled 116 men with prostates ranging up to 80 cubic centimeters. The second trial, WATER II, launched in 2017 and enrolled 101 men with prostates ranging between 80 and 150 cubic centimeters. (Normal prostates range from 25 to 30 cubic centimeters in size.) Enrolled patients had a median age of 66 in the WATER study and 68 in WATER II. In addition, 92% of men in the WATER trial were sexually active, as were 75% of the men in WATER II.
Both clinical trials used the so-called International Prostate Symptom Score (IPSS) to measure treatment-related improvements in urinary functioning and quality of life. Calculated based on how patients rate their symptoms on a standardized questionnaire, IPSS scores fall into three categories: mild symptom scores range from 1 to 7; intermediate symptom scores range from 8 to 18; and scores greater than 19 indicate severe symptoms.
When they first enrolled in the trials, men in the WATER and WATER II studies reported average IPSS scores of 22.9 and 23.3 respectively. Five years later, the average respective scores were much lower: 7.0 and 6.8. The average length of hospital stay was 1.4 days in the WATER group and 1.6 days for the WATER II group. Only 1% of men were taking BPH medications after five years, and fewer than 5% had been surgically re-treated.
Another randomized control trial, WATER III, is currently underway in Europe. That trial compares aquablation with a more established type of BPH surgery, prostate enucleation, which uses a laser to remove obstructing tissues. Six-month data reported in 2023 showed that men in either group had comparable symptom improvements.
However, 98% of men in the prostate enucleation group had ejaculatory dysfunction. That side effect is caused by damage to delicate tissues around the bladder neck that propel semen out of the body. Semen therefore flows back into the bladder, a condition called retrograde ejaculation. None of the men in the aquablation group reported ejaculatory problems.
A word of caution
Aquablation can result in extended bleeding, cautions Dr. Heidi Rayala, an assistant professor of urology at Harvard Medical School and a member of the Harvard Medical School Guide to Prostate Diseases advisory board. That’s because unlike other types of surgery for BPH, including prostate enucleation, aquablation doesn’t cauterize tissues with heat. “I tell my patients to expect some blood in the urine for about four to six weeks after the procedure,” Dr. Rayala said.
Moreover, aquablation may be unsuitable for some men who take blood thinners to prevent blood from clotting, according to Dr. Rayala. Appropriate candidates for the surgery must be able to “safely discontinue anticoagulant medications during post-operative healing, given the bleeding risk,” Dr. Rayala said. Still, aquablation is an excellent option for most men, Dr. Rayala said, especially those with medium to large prostates “who want a durable solution with a lower risk of sexual side effects.”
“These early results are encouraging, but limited by a relatively small number of patients,” said Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases. “Further evidence with a significantly larger number of patients and longer follow-up will help to support this new method of reducing prostate tissue as an important treatment option.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD